In sharper focus
Take a 40-year-old problem of ‘unfocused’ ultrasound images, add dedicated researchers at a centre for research-based innovation, and the result? Sharper, clearer images regardless of the patient’s anatomy – a vitally important improvement for diagnosing heart attacks and their severity.
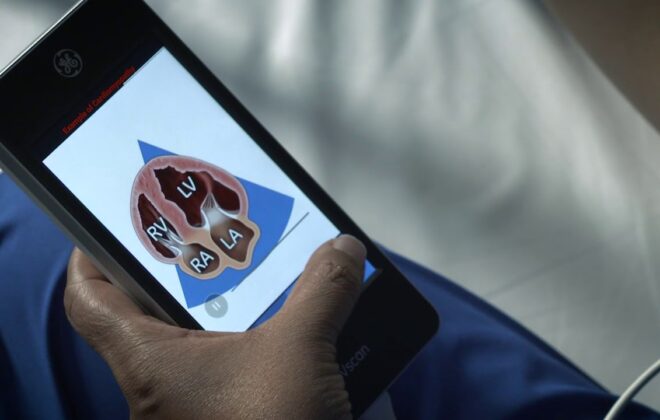
When diagnosing heart attacks, subtle changes in movement in the heart muscle can give information on the size of the attack and the extent of muscular damage. In most cases, this can be seen by an experienced sonographer, but in 10-15% of patients, image quality is suboptimal. Not a high percentage you think? Add then that more than 100 million ultrasound heart examinations are carried out globally every year, and the magnitude of the challenge can be overwhelming.
“Having ultrasound pass through the body wall can be compared to light travelling through a layer of Vaseline on your camera lens – it results in a blurred image with poor contrast. The image is said to be aberrated,” CIUS centre director and researcher Svein-Erik Måsøy explains.
A window in the wall
The challenge lies in the fact that the human body consists of various substances such as fat, muscles, tissue and bones, that the sonographer and the soundwaves from the ultrasound probe have to navigate. And no two human beings are identical.
This is why in 2017, CIUS researchers at GE Healthcare, NTNU, University of Oslo and St. Olavs hospital came together to solve the 40-year-old issue of aberration. The result is the Adapt technology:
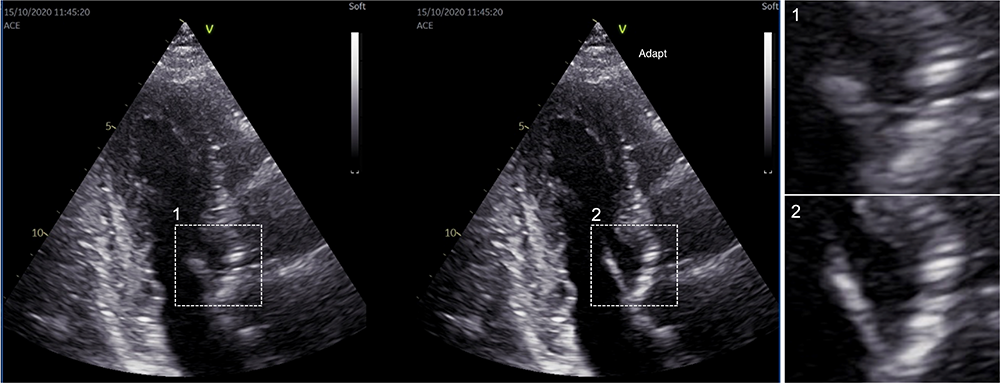
“Adapt is an algorithm that uses the recorded ultrasound data to estimate and compensate for the effect of the body wall in each individual patient. It adapts itself to the patient making more than 100 corrections to each image pixel per second,” Måsøy says.
It was tested in a pilot study with four clinicians at St. Olavs hospital, and the result was that Adapt was preferred in 97% of cases compared with ultrasound scans without the new technology, and it has already been made available on the GE Vingmed Vivid E95 scanners worldwide.
“Adapt sharpens images, increasing contrast resolution and improving diagnostic confidence,” says Echo technician Lill Merete Skretteberg Lindøe at Oslo University Hospital. “The imaging enhancements reduce non-diagnostic images and improve productivity and workload by reducing scan time and improving ergonomics.”
A gam(ing)-changer
So how come it suddenly only took five years of dedicated CIUS research to solve the 40-year-old problem? Well, that is something we can thank the gaming industry for – at least partially!
“Advancements in GPU processing power over the past decade, brought to the fore by the gaming industry and recent improvements in 3D ultrasound probes, have been instrumental for the success of Adapt,” Måsøy says.
“Modern ultrasound systems have moved ultrasound image reconstruction from dedicated hardware chips to software using GPUs, allowing for storage of so-called raw-unprocessed ultrasound data. This data can be used to recreate images by testing variations of algorithms over and over again on realistic, clinical data. This was simply not possible before, and therefore represented a game-changer in the possibilities for making Adapt work.”
But to create the algorithm, the research team consisting of 10 core members and many more contributors, started studying more than 40 000 ultrasound images of the heart. This was to understand the fundamental mechanisms needed to make the algorithm work – regardless of the great variations in patients’ body walls.
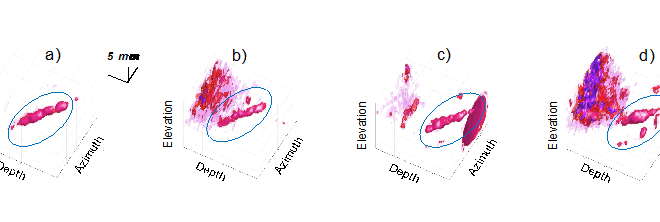
Unlike traditional methods, which rely on a mathematical model of how ultrasound waves move at a constant speed through the body, the Adapt algorithm optimises the image reconstruction process for each individual patient. This adaptive approach takes into account the unique anatomy of each patient, allowing for real-time adjustments to the ultrasound image formation process.
“At GE HealthCare, we are committed to creating a world where healthcare has no limits, and the development of the Adapt technology serves as a shining example of this mission in action,” explains Bastien Dénarié, Manager of External Imaging research at GE HealthCare.
“This innovative technology, developed in partnership with the CIUS team, improves ultrasound image quality to an industry-leading level. This would not have been possible without the excellent cross-disciplinary collaboration between researchers and clinicians that is so unique to CIUS. The Adapt technology’s ability to adapt to the unique characteristics of each patient’s anatomy is a game-changer for the diagnosis and treatment of heart attacks. We are proud to have been a part of this breakthrough and look forward to continuing our collaboration with CIUS to push the boundaries of medical technology and improve patient care.”
The Adapt technology
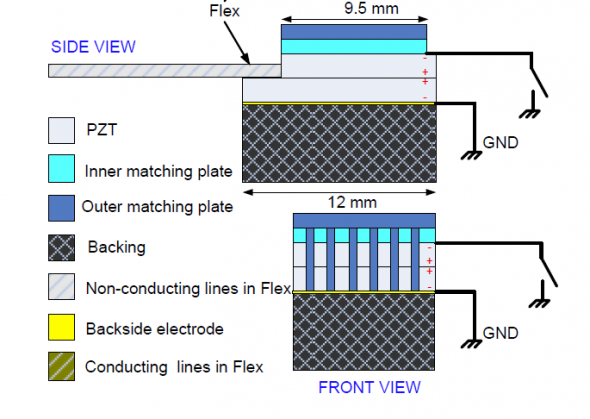
Ultrasound images are formed by sending a concentrated ultrasound wave into the body and recording the returning echoes. This is done by using a probe acting simultaneously as a speaker and microphone. The probe has many elements (thousands) which allow the system to locate precisely where the echoes are returning from by logging the arrival times of each ultrasound signal at each element. By comparing arrival time differences across all elements, the exact position of each individual echo can be found.
This process works perfectly if tissue is even. But the body wall is not even creating additional unknown varying arrival times across the probe’s elements. This is the basic mechanism for reduced image resolution and contrast. The system can no longer work out the exact location of each echo.
Adapt works by estimating the change in arrival times for all the elements of the probe and compensates for this in the image reconstruction process, thereby improving the echo localisation process and consequently providing better images.
This article first appeared in the 2022 CIUS Annual Report.
-
Kari Williamsonhttps://www.ntnu.no/blogger/cius/author/kari_williamson/
-
Kari Williamsonhttps://www.ntnu.no/blogger/cius/author/kari_williamson/
-
Kari Williamsonhttps://www.ntnu.no/blogger/cius/author/kari_williamson/
-
Kari Williamsonhttps://www.ntnu.no/blogger/cius/author/kari_williamson/