Promising marker for detecting disease activity in microscopic colitis
Microscopic colitis (MC) is a distinctive and lesser-known subtype of the inflammatory bowel diseases (IBD). It is characterized by chronic and watery diarrhea without blood and can be very socially disabling. Many patients are incorrectly diagnosed with «irritable bowel syndrome» (IBS) and, thus, are not offered the right treatment for MC that for the vast majority is very effective.
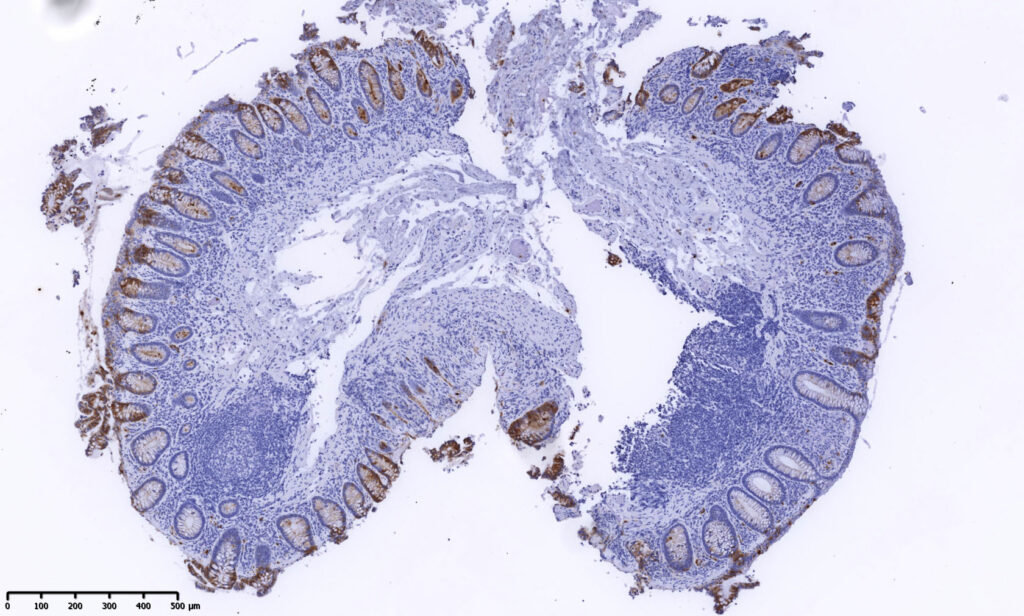
The diagnosis is dependent on detecting changes in tissue samples from the colon. Such samples can only be taken by colonoscopy. In MC, the pathologists will find either increased thickness of collagen under the surface epithelium (Collagenous colitis), increased infiltration of the inflammatory lymphocytes in the epithelium (Lymphocytic colitis) or a combination of this (Incomplete colitis).
These microscopic changes in the intestinal mucosa do not reflect improvement in symptoms after successful treatment. Until now, there are no non-invasive biomarkers that say anything about disease activity in MC, and there is also a need for supplementary tools to make a more reliable microscopic diagnosis.
Neutrophil gelatinase-associated lipocalin (NGAL) is a stable protein that is induced by inflammation. NGAL differs from other biomarkers (for example calprotectin and lactoferrin) also found in the neutrophilic inflammatory cells, since NGAL additionally is induced in the epithelial cells. Therefore, NGAL has potential as a biomarker beyond these already established markers in both neutrophilic and non-neutrophilic mucosal inflammation, and it can be measured in both blood, intestinal mucosa and feces.
We are the first to show that NGAL increases in the epithelial cells in the colonic mucosa during active MC and that the amount reduces almost back to normal with successful treatment. This change is also reflected and can be measured in the patients’ stool.
This increase is not seen in other diarrheal conditions such as IBS. The changes in NGAL was more consistent with the patients’ clinical condition and diarrhea than with the other microscopic changes in the mucosa that are typical of this diagnosis.
We therefore suggest that NGAL in the epithelium may be a complementary tool for pathologists in the microscopic diagnosis of MC, as well as a new clinically relevant biomarker for disease activity in MC and to distinguish this patient group from both those who are healthy and have IBS.
Publication
Mucosal and faecal neutrophil gelatinase-associated lipocalin as potential biomarkers for collagenous colitis.
Bakke I, Walaas GA, Bruland T, Røyset ES, van Beelen Granlund A, Escudero-Hernández C, Thorsvik S, Münch A, Sandvik AK, Østvik AE.J Gastroenterol. 2021 Oct;56(10):914-927. doi: 10.1007/s00535-021-01814-y. Epub 2021 Aug 19.PMID: 34414506

Ingunn Bakke
Associate Professor,
Department of Clinical and Molecular Medicine, NTNU
-
This author does not have any more posts.

Ann Elisabet Østvik
Postdoctoral Fellow,
Department of Clinical and Molecular Medicine, NTNU
-
This author does not have any more posts.

CAG IBD – Precision medicine in inflammatory bowel disease
CAG-IBD is a Clinical Academic Group (CAG) aiming to unify research on inflammatory bowel disease and development of clinical skills across university, hospitals and clinical departments, and groups of healthcare workers in Central Norway.
-
This author does not have any more posts.



