Uncovering stiff or leaky heart valves
Modern ultrasound scanners combined with technological developments at NTNU may improve diagnostics for diseases related to narrow or leaky heart valves. Advanced 3D Doppler and high frame rate imaging makes it possible to visualise cardiac flow and minor movements of the heart’s muscular tissue more precisely, according to PhD Candidates Torvald Espeland and Erik Andreas Rye Berg.
Torvald Espeland’s research aims to detect increased stiffness of the myocardium (the muscular tissue of the heart) in patients with valvular heart disease. He is optimistic about the results. His colleague Erik Andreas Rye Berg has taken on the challenges of developing better methods to quantify leaks in heart valves.
Visualising the velocity
Espeland is researching the detection of scar tissue (fi- brosis) in the myocardium: “Until now, scar tissue has only been detectable using MRI. Some mechanical waves in the myocardium travel very fast, and the velocity of these waves depends on the stiffness of the myocardium. These waves are now easier to visualise with the newest ultra- sound scanner and software developed here at NTNU,” explains Espeland.
He has examined 100 patients with a narrow heart valve – aortic stenosis. The patients complete questionnaires, undergo a clinical examination, a walking test and electrocardiograms, and provide blood samples.
“We perform a thorough conventional ultrasound examination on each patient in addition to the newest, more advanced methods that we aim to investigate. All participants undergo a cardiac MRI,” says Espeland. They analyse the results to see how well echo performs compared with MRI in detecting scar tissue.
“So far, the new method seems feasible, meaning that it is possible to perform these acquisitions,” says Espeland.
Who needs surgery or an intervention?
Patients with aortic stenosis may undergo open-heart surgery or a catheter-based intervention when the heart valve is severely narrowed and they experience symptoms or demonstrate reduced heart function. The typical symptoms will be shortness of breath, chest pains, or fainting during exertion.
“Some patients don’t report symptoms at their regular check-ups. When investigating this more, you may discover that they have stopped doing activities they previously enjoyed,” says Espeland. One possible reason for this under-reporting could be the slow development of the symptoms.
Every year, almost 500 patients at St. Olavs hospital are evaluated for aortic stenosis intervention.
“Lately, a lot of research has focused on examining which patients have worsened prognosis without the traditional symptoms or reduced pumping function. My research adds to that, trying to predict which patients need earlier intervention,” says Espeland.

Assessing leaking valves
A leaky heart valve causes some of the blood to flow in the wrong direction. If this valvular regurgitation is severe, the patient may need surgery. It is essential to have an exact method to quantify the leak. Currently, the assessment relies on the integration of many methods and parameters, each with its own strengths and weaknesses.
Erik Andreas Rye Berg’s research is based on a method developed at NTNU almost 15 years ago, which gave good results but was too complicated to perform in daily clinical life.
“Now we have tried to come up with a simpler method more suited for automated analysis,” says Rye Berg.
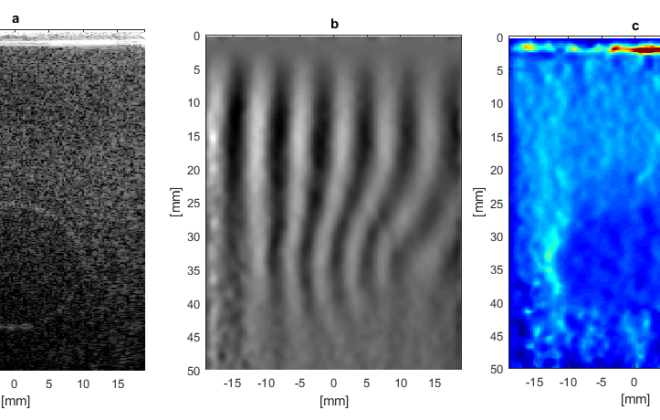
He explains that while they previously fired many separate ultrasound beams and aggregated them, they now shoot one broad ultrasound beam.
“By firing all the ultrasound elements simultaneously up to 20 000 times per second, we record a cube containing detailed velocity information from the regurgitant jet. This way, we can assess both the volume and area of the regurgitation.”
Lab vs. reality
Initial testing in patients gave promising results. After that, the success rate sank. There are two major problems with the technology: limitations in recording of the highest velocities in some patients, and undesired narrowing of the ultrasound beam. In addition, all the ‘noise’ created by the human body makes it much harder to use the method in real life than in the lab.
“On paper, this is thrilling. In the lab, the results are good. In the patients, we haven’t succeeded yet,” Rye Berg concludes.
“Fortunately, I have several projects I am working on in my PhD,” he adds. “We are publishing one or two articles on this, because we should tell the world that this is how far we have come, but unfortunately it doesn’t work in the patients yet.”
As experienced medical doctors, they started their PhD work in 2017 and plan to complete it during 2022, with Svend Aakhus as their supervisor and GE Vingmed Ultrasound as the industrial partner.
This article first appeared in the 2021 CIUS Annual Report.
Wenche Margrethe Kulmo
-
Wenche Margrethe Kulmo#molongui-disabled-link
-
Wenche Margrethe Kulmo#molongui-disabled-link
-
Wenche Margrethe Kulmo#molongui-disabled-link
-
Wenche Margrethe Kulmo#molongui-disabled-link